
- Posted
- Categories
-
- OpenPrescribing
OpenFormulary: ahead of its time
In 2019, we pitched a national tool to track local formularies. Now the NHS is doing just that! We’re sharing our plans and advice to help it succeed.

In 2019, we pitched a national tool to track local formularies. Now the NHS is doing just that! We’re sharing our plans and advice to help it succeed.

A summary of our discussion with NHS leaders on how Medicines Optimisation teams can leverage data science to enhance their strategic capability.

Bennett research integrity lead, Nick DeVito, on the encouraging words about code sharing that Kamran Abbasi delivered at our recent OpenSAFELY Community Symposium.
Details on two new papers from the Bennett Institute Research Integrity Team.

The first session in the Bennett Conference discussed past and present work of the Institute on research integrity and policy issues.
The Clinical Trial Information System (CTIS) is the European Union’s new registry set to fully replace the existing EU Clinical Trials Registry next year. Nick DeVito decided to take a spin through the registry and record some of his initial thoughts.

In June 2022, the NHS published its new data strategy Data Saves Lives. The strategy is a broad ranging document, covering seven ‘key areas’.

Building a strong case for the broader adoption and use of Trusted Research Environments across the NHS.

An overview of the UK Government’s nine data policy documents published April - July 2022.

Today the NHS has published the final version of it’s “Data Saves Lives” strategy, setting out its key commitments in seven key areas
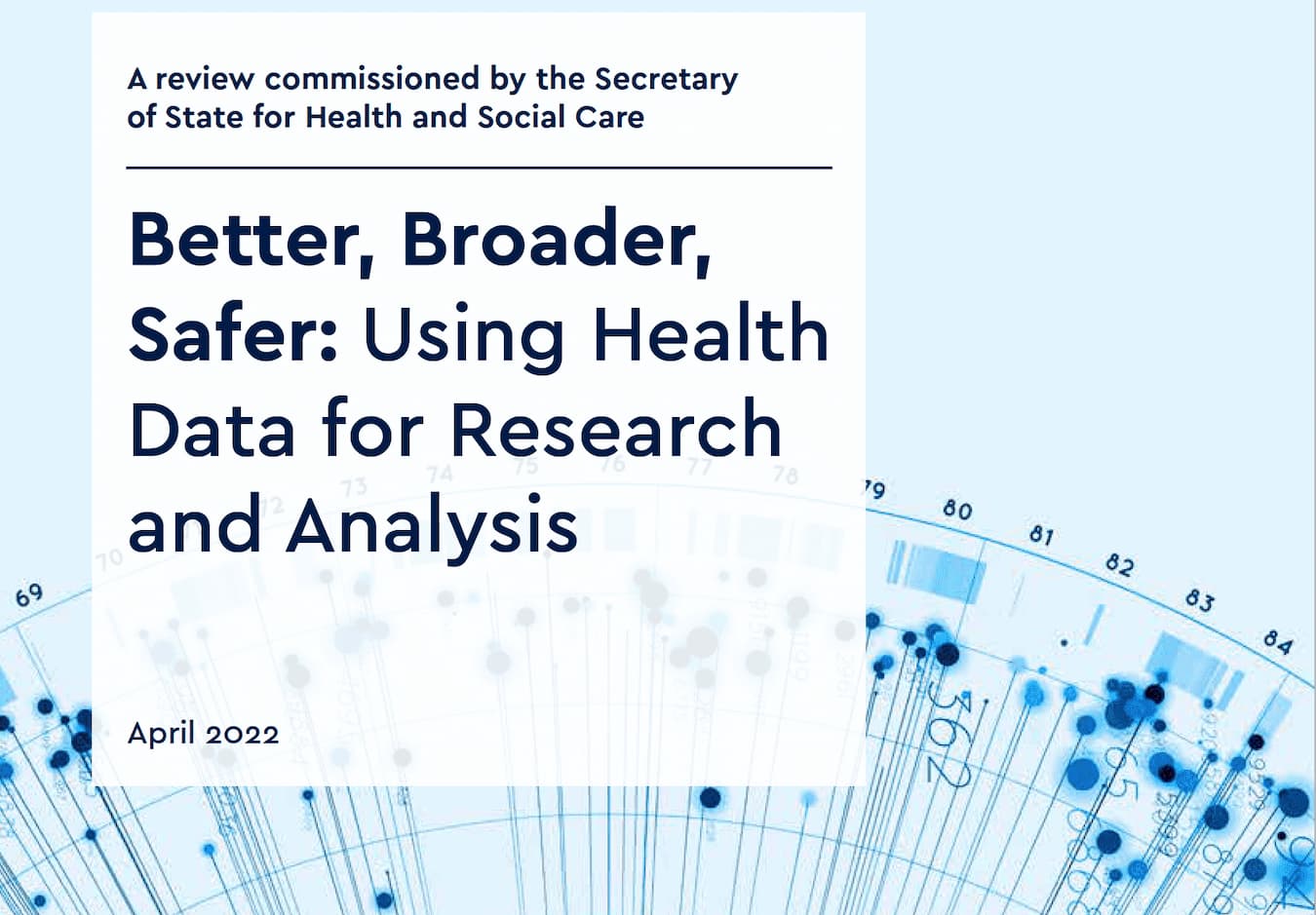
Over the past year Ben and our policy lead Jess, have conducted interviews with over 300 individuals, held 8 open focus groups, reviewed over 100 written submissions, and conducted extensive desk research, to reach the conclusions that were published yesterday in the Goldacre Review.

This week sees the publication of an independent Citizens’ Jury commissioned for NHSx and the National Data Guardian which found that OpenSAFELY was by far the most strongly and consistently supported of all NHS COVID data projects examined.

On our first anniversary, from the Policy Lead in the Bennett Institute, this is the brief story of the positive side from all our lives: how OpenSAFELY came to life, and what we’ve achieved so far.

This is a draft discussion paper, the first of a series exploring “open team science” approaches to managing health data, and specifically how to create a collaborative computational data science ecosystem where the sharing and re-use of objects such as codelists and code is facilitated, encouraged, recognised, and rewarded. As a microcosm of this we have first explored “codelists”. There are currently no ‘answers’ or preferred solutions given. We will be holding an open discussion with the research community on 2nd March at 3pm - you can book to join us here.

We have been very busy since our last newsletter back in July and there are tonnes of exciting updates for you here!
The Faculty of Pain Medicine has recently updated their recommendation on oral morphine equivalence (OME) which we use on our OpenPrescribing measure of OME. We have taken this opportunity to update and a new novel implementation of how we assess OME. Until this work is completed we have taken the decision to “suspend” the measure from dashboards however you can still view the old method using this link.

In July, Ben and Brian wrote a piece in the British Medical Journal arguing that hospital medicines data should be openly shared. Magnificently, the NHS has now made secondary care medicines data (SCMD) available. You can read the full technical specification of the data here but briefly: it is hospital pharmacy stock control data, which is collected and processed by Rx-Info, and is now published on the NHS Business Services Authority website in the NHS dm+d standard we know, love, and have documented well.

Working on behalf of NHS England we have now built a full, open source, highly secure analytics platform running across the full pseudonymised primary care records of 24 million people, rising soon to 55 million, 95% of the population of England. We have pursued a new model: for privacy, security, low cost, and near-real-time data access, we have built the analytics platform inside the EHR data centre of the major EHR providers, where the data already resides; in addition we have built software that uses tiered increasingly non-disclosive tables to prevent researchers ever needing direct access to the disclosive underlying data to run analyses; code is developed against simulated data using open platforms before moving to the live data environment. Everything has run smoothly. We are fully live inside TPP; we are signed off with full data access and end-stage tech development for the computational platform with EMIS.

It has been a busy month for paper publication at The Bennett Institute. We have written a brief description of the most recent papers below. Please sharewith colleagues and get in touch if you have any relevant observations! Remember you can read all our academic papers related to OpenPrescribing on our research page.
Hospital medicines data: We are frequently contacted at OpenPrescribing about when we are going to make a hospital version. Unlike primary care, access to hospital medicines data is restricted. The BMJ have just published our Bennett Institute article about why we think The NHS deserves better use of hospital medicines data.

This week the British Journal of General Practice published our latest paper on unsafe prescribing of methotrexate. We found that the prevalence of unsafe methotrexate prescribing (10mg tablets) has reduced but remains common, with substantial variation between practices and CCGs. In the paper we also discuss recommendations for better strategies around implementation.
Anyone can view the live data on unsafe methotrexate prescribing at openprescribing.net/measure/methotrexate, to support audit and review in your local organisation. Read the paper here and you can watch Dr. Kevin Barret (twitter @drkbarret) describe here how his practice used OpenPrescribing to identify a breach of their practice policy on methotreaxte prescribing and fix it!

OpenSAFELY is a new secure analytics platform for electronic health records in the NHS, created to deliver urgent results during the global COVID-19 emergency. OpenSAFELY is a collaboration between the Bennett Institute, the EHR group at London School of Hygiene and Tropical Medicine and TPP who produce SystmOne. OpenSAFELY is now successfully delivering analyses across more than 24 million patients’ full pseudonymised primary care NHS records. The first analysis from OpenSAFELY is Factors associated with COVID-19-related hospital death in the linked electronic health records of 17 million adult NHS patients with more answers to important questions expected shortly.

Covid-19 shows that we must overcome organisational barriers to deliver clean, realtime, standardised data in support of direct care, system planning, and urgent response

Most people share their end of year roundup during late December when everyone is too full of cake to read. Now you’re back in the saddle, here’s our roundup of everything the Bennett Institute threw out into the world over the previous 12 months!
OpenPrescribing.net went from strength to strength, with over 135,000 unique users last year. We now have over 80 measures of prescribing safety, efficacy and cost-effectiveness and have been working on new types of measures and alerts to identify “outlier” prescribing, such as with zuclopenthixol. In 2019 we also: launched new dashboards and bespoke alerts for every single primary care network (PCN), sustainability and transformation partnership (STP), and NHS region; upgraded the Analyse page to support more organisations with bespoke medicines queries; and developed tools to help solve the problem of Ghost Branded Generics which cost the NHS an extra £11.6million per annum but has massively reduced during 2019.

We have now launched our long-awaited Primary Care Networks (PCNs) dashboard, made possible thanks to the the membership list being published by NHS England last week.
We have PCN prescribing dashboards for every single NHS PCN and their member general practices. (Don’t know your PCN’s name? You can find it on your practice dashboard). This allows anyone to explore NHS prescribing patterns in their PCN and how this compares to others across England — supporting safer, more efficient prescribing.
Our EU TrialsTracker has been assessing compliance with EU trial reporting guidelines for over a year now. Our data has been used by Parliamentary Committees and trial sponsors to improve the reporting of clinical trials registered on the EU Clinical Trials Register (EUCTR).
We previously shared some of the data issues that make complete assessments of trials on the EUCTR difficult. One particularly troubling issue is dealing with trials that never began. Sometimes trials get all the necessary approvals to begin, and therefore are automatically registered on the EUCTR. In rare instances, and for any number of reasons, they then simply never begin; they are cancelled before they enroll a single participant or collect any data. Obviously, these trials have no results to report.

Last week, the Commons Science and Technology Select Committee convened an inquiry following-up their previous clinical trials transparency efforts. The Select Committee has been very active in the trials transparency space over the past two years. Earlier this year they sent letters to every public university and NHS trust in the UK that sponsors clinical trials on the EU register. These letters reminded sponsors of their trial reporting responsibilities and provided them with reporting performance figures based on data from our EU TrialsTracker.


Our newest paper is now out in the BMJ! Here we show huge variation in adoption of warranted changes in prescribing behaviour, using some exciting new openly available change detection methods.
This month we have launched a range of new measures. As always, measures are prioritised on your dashboard by potential for improvement so you can quickly and easily spot where your organisation is an outlier. You can also sort by potential savings or group measures by clinical condition.

Following many requests from users, we have created links from our measures to the corresponding search on the Analyse page. This is particularly useful if you want to see multiple practices or CCGs on one chart, view the results on a map, or see exactly which products are included in the measure.
You will notice this is not yet available for all of our measures (which now number close to 100), due to the complex way some measures are constructed. This currently affects just 12 of our standard measures and 4 of the Low-Priority prescribing measures, and we hope to keep increasing the options in the coming months.

This week we have launched a new browser for the NHS Dictionary of Medicines and Devices, better known as dm+d. dm+d is the standard dictionary for the medicines and devices used across the NHS. At last count there were over 150,000 packs of medicines and devices described. You can read more about the dm+d in [this detailed blog]/blog/2019/08/what-is-the-dm-d-the-nhs-dictionary-of-medicines-and-devices/).
We have been using the dm+d browser internally for a while, and having found it very useful we believe it will come in handy for others too, so we have now made it available publicly for anyone to use. Read more about the tool here.

Earlier this year we noticed a disturbing trend among UK trials registered on the EUCTR. The amount of newly approved and registered trials on the EUCTR dropped drastically following the 2016 Brexit vote. The chart from that blog post (from May 2019) is included below.

When we reached out to the MHRA to ask about this, they stated that there was actually no decline in UK trials post-Brexit but rather administrative delays that kept trials from appearing on the public-facing EUCTR website. They noted this issue was being addressed and updates would be completed by the end of Q2 2019.

Yesterday (27 June), NHS England completed its consultation on an additional proposed set of products being considered for a recommendation against regular use in primary care. Therefore, on the site we have now included these new items in the set of low-priority measures. The newly added products include bath and shower emollients, higher cost insulin pen needles and dronedarone. See how your practice or CCG is performing on these measures here, or navigate to the Low Priority measures from your favourite organisation’s dashboard.


One of our recent papers, published in the Journal of Antimicrobial Chemotherapy, highlighted variability in the speed at which different CCGs switched from prescribing trimethoprim to nitrofurantoin (as recommended by PHE for uncomplicated UTI).
It appears that the practices which changed the most were in CCGs that had taken some action to promote the new guidelines, such as a change in formulary. What are the implications? Read more on this in our blog and you can of course see any region’s performance on this measure on OpenPrescribing.

We recently noticed a very dramatic drop in the number of UK clinical trials post-Brexit on the EU Clinical Trials Register (which would be a catastrophe for British science) and wrote to MHRA to get their view. It turns out that the drop is largely due to bad data management: this is worrying, but not the same thing as a drop in the number of UK clinical trials.
We’ve been conducting research on trends in clinical trials globally with one very striking recent finding: examining clinical trials on medicinal products, using the EU Clinical Trials Register (EUCTR), the number of trials with a competent authority decision from the UK has fallen dramatically. As you can see on the graph below: from a long-term trend of around 150 new trials per quarter, after 2016 there is a rapid drop to fewer than 50, and now fewer than 10.

We have introduced a new email alert service, built upon our recently-launched NHS Price Concession calculator, which shows the cost impact of concessions for every single practice, CCG and for all of England combined.
If you sign up for these new alerts, an email will pop into your inbox soon after a new price concession is announced (approximately once per week) to update you on the impact these costs are predicted to have on your practice/CCG. Read more in our blog, or sign up by going to the price concessions tool from your practice or CCG dashboard.
As you know, here at the Bennett Institute we are working on the RetractoBot project to reduce the number of cited retracted papers.
Citations of retracted RCTs are particularly dangerous because such trials provide strong and unbiased evidence of treatment’s safety and efficacy (hierarchy of evidence). Moreover, results of RCTs are often pooled in systematic reviews and meta-analyses, which are used to synthesise the available evidence on a given subject or to justify clinical guidelines.

Now that we’ve launched our FDAAA TrialsTracker, we plan on occasionally taking a closer look at some of the trials that go unreported. Our first blog was about a trial examining 2 drug combinations for managing pain during labor (NCT01846221).
So why do we think this specific trial is due to report? While we go through how we established our criteria and set up our database in detail in our preprint paper on Biorxiv, we wanted to walk you through exactly what fields matter on ClinicalTrials.gov and how we used them to build our tracker. We think we were able to do this well, but are open to feedback and will amend our paper and methods as necessary.

At OpenPrescribing, we provide tools for analysing prescribing behaviour in primary care in the NHS in England. If you work with prescribing data, you may have noticed that practices which are “dormant” apparently continue to prescribe. This short article explains why, for the curious.
Our prescribing data comes from the NHS Business Services Authority (NHSBSA), who are responsible for processing dispensing information supplied by pharmacies. Each line of the data includes a practice code which uniquely identifies the GP Practice that issued the prescription. To understand more about each practice (including its contact details, location, and CCG membership), we cross-reference this code with GP Practice data published by NHS Digital. That data contains a column, status, which sometimes contains the value D, for dormant.